Over my career, I have seen countless patients whose lives have forever been changed for the better with a hip replacement. This is one of the most successful surgeries ever devised. In spite of these positives, there are some ongoing concerns about what activities people can do after a hip replacement.
The restrictions on hip replacement can be divided into early and late restrictions. One other important point: Some patients come to us and say that their surgeon told them that they do not have restrictions. All surgeons are limited by the materials available on the market today. Those surgeons who have less restrictions may be operating under a policy of generalized optimism. Some of these restrictions are guided by experience rather than scientifically proven data.
My approach is to think of the long-term payoff for short term sacrifices. The complications we are trying to avoid with restrictions are fractures of the bone, loosening of the implants, dislocations of the hip replacement and infections.
Let's discuss each of these separately. Most hip replacements we are currently performing are done so through an anterior approach. The prostheses we use are usually made of titanium. Titanium is a wonderful surface for hip replacements because it is flexible, just like the bone. The bone cells also love titanium, since a rough titanium surface feels like a bone surface to them and they actually fuse the bone to the titanium over the course of six to eight weeks. The femur or thigh bone has to be carefully exposed and brought up in such as a way as to avoid putting in the prosthesis at the wrong angle. When this is not done properly, the bone can break. Even when done properly, sometime the bone is soft due to osteoporosis and can crack. We carefully inspect the femur at the end of each surgery to be sure there is no crack. If a small crack is seen we augment the bone with metal wires or cables. It is important in general to put only the weight specified by your surgeon on the leg. In some cases, if the bone is very weak, we may restrict weightbearing to 30 pounds. This can be assessed by the patient putting their leg on a scale to understand what 30 pounds will feel like on the bottom of their heel. Alternatively, 30 pounds can be estimated by telling the patient to pretend like they are walking on "eggshells." We continue this for approximately six weeks after surgery to give the implant a chance to heal to the bone. After that point, we let patients put their full weight on the leg. In most cases, we tell patients that they can put their entire weight on the leg and that makes the recovery even easier. So the take-home point is to follow the instructions provided by your surgeon.
The second complication we try to avoid is loosening of the implants. This can happen when patients do too much walking and stress the implants prior to the ingrowth process. Generally, I advise patients to walk only a few hundred yards a day total until they get to around six weeks. By that point, the implants are ingrown with bone, meaning that the bone is fused to the implant.
Dislocations used to be a very big concern for hip replacements. Our native joints have a suction cup effect, meaning that even when a patient is under full anesthesia, one cannot easily separate the joint due to this effect. An artificial joint like a hip replacement does not have that effect due to the nature of hard materials like plastic, metal and ceramic. The anterior approach has really reduced the rate of dislocations since the muscles that stabilize the hip from the back (the piriformis, the gemelli muscles, and the quadratus femoris... for the anatomy buffs) are not cut. This leads to an inherently stable hip. Even with the posterior approach, the repairs that we do can often protect the hip. However, for all approaches, it is important to avoid extremes of motion after hip replacement. What do I mean by the extremes of motion? That is really a subjective term. I tell my patients that they should never try and get their hips super flexible. Achieving a high level of flexibility can stretch out the joint covering called the capsule, the ligaments and the tendons that keep the artificial hip in its socket. I typically recommend avoidance of bending the hip more than around 90 degrees (a right angle) for the first six weeks and 130 degrees (a six-inch gap or less between the knee and the chest) thereafter. I also recommend always having the knee of the surgical leg pointing outward with any bending. That means if you are picking up something off the ground, have your knees always going outward. This is the safest position for the hip replacement. In spite of all of these measures, hip replacements can still dislocate. This can be due to other factors like implant positioning, soft tissue laxity or stretchiness, or decreased flexibility in the spine. Dislocations are painful and dangerous. They usually require an urgent trip to the emergency room and anesthesia to put the hip "back in." As a result, the best thing is to avoid them if at all possible by following the instructions of your surgeon.
No Leg Crossing
For at least two months after hip replacement surgery, avoid crossing your legs. This is particularly a risk if you bring your knee across your body. Putting a pillow between your legs while sleeping can prevent inadvertent leg crossing during sleep.
No Sleeping on Your Stomach
Sleeping on your stomach can cause the hip to twist, which raises the risk of dislocation. Also avoid lying on the side of your body affected by the surgery. This puts a lot of stress on the implant since your entire body weight is now loaded on the hip replacement. For the best results, sleep on your back. This also prevents inadvertent crossing of your legs during sleep Another sleeping tip: Do not reach down and pull up the blankets as you may in effect be bending down too much.
No Low Chairs
Stay out of low chairs while recuperating. The same holds true for overstuffed or soft furniture. Getting in and out of each of these could cause a momentary high degree of bending of the hip which can lead to dislocations. Having a bedside commode or raised toilet seat can also help in avoiding high bending at the hip. If possible, try and sit on firm chairs with armrests and straight backs. Always keep your knees below your hips.
Use Long-Handled Reachers
Reaching for items is best avoided during hip replacement surgery recovery. This action causes excessive bending. Instead, use long-handled reachers for grasping. These are available at medical supply stores or through your physical therapist.
Do Not Step Into a Car
Avoid stepping into a car while recuperating. Make sure the car is parked on a flat area, and that the front passenger seat is pushed back as far as possible. Use the walking device recommended by your doctor. Once next to the car, turn and back up to the front passenger seat. Place your right hand on the door frame and your left hand on the seat or dashboard. Carefully lower yourself in.
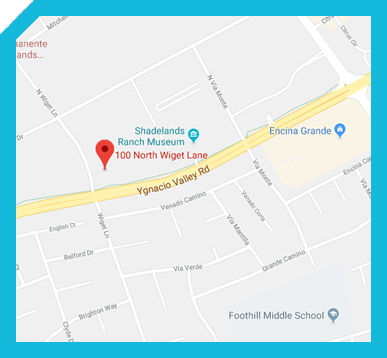
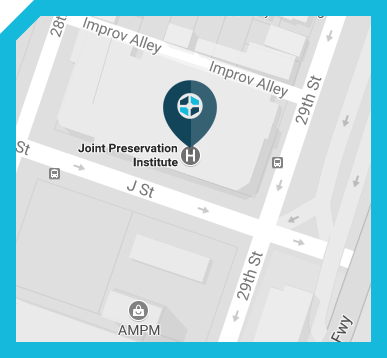
Contact Us
If you are experiencing hip problems, contact the Joint Preservation Institute today by giving us a call, or email us at Joint Preservation in Sacramento or the San Francisco Bay Area. If hip replacement surgery is necessary, Dr. Jamali will answer all of your questions and discuss your options.




 Activities to Avoid After Hip Replacement
Activities to Avoid After Hip Replacement